Updated on Nov 2021: 6.5 years after Brain Surgery
This is the current status of my symptoms in the order of relieved – mostly relieved – on-going but may be relieved – may not be relieved.
When I say relieved, I mean the symptoms don’t occur on a daily basis and that the frequency, severity, and duration are reduced to a drastic extent but do come up when my body or brain is under a lot of stress. Please note that brain injury causes trauma in the body that might take a while (undefined!) to recover. It is a continual process that requires the person with a brain injury to regulate and be mindful of physical and mental activity. I know logic says that I got fixed and so I should run at the optimal speed but the human body is a very complicated thing to mend.
I was told that it might take anywhere between 3–10 years for my body to feel as if no intrusion took place. For now, it’s still recovering from the shock of my pineal gland going on a sabbatical. Apart from symptoms of the brain tumor, I experience problems from the injury caused by surgery and the side effects of medication. At this point, it is very hard to point out the cause of each symptom. I’m very attentive to what my body (my brain tells it obviously!) needs, for example, if it says you can’t walk anymore, I just stop and take a cab back home. I try but find it challenging to be mindful of any new symptoms when I begin a new medication.
It’s very important to listen to your body and learn to differentiate the signals it is giving you. It is very easy to confuse chronic fatigue with laziness, lethargy with a lack of motivation, and comprehension problems with lack of focus. These were the initial symptoms I couldn’t understand and didn’t pay attention to. Also, let nobody come between you and your body. Let nobody tell you that you should or should not experience a certain symptom. Your body is unique and statistical significance should not convince you to feel a different way or play a part in your diagnosis.
Inability to process information
I’d go to this cafe beside my house every other day because they had delicious food for every day I got bad news (which was more often than every other day). Their menu is half a page (5-6 pages) and I’d ask them every time I visit what they recommend. It had to get old at some point! I couldn’t read a menu, stack the items in my mind and compare them mentally. I needed help with everything that needed processing information. It would take me forever to decide which tea I wanted to drink from my kitchen (I do have a few more than usual but that’s not the point). Pictures weren’t of much help either. Ayan, my punchbag ;), would say, “Don’t look at the menu. Just tell me what you want.” I’d him something like tangy fish soup with bamboo in it. If he didn’t find it on the menu, he’d find another restaurant to go to :). It would have been impossible to navigate without people who did not resent me for how dependent I was on them. I needed someone to help me cross the road when the pedestrian signal was on.
I caught myself standing in the middle of a road with vehicles honking at me at least twice before I realized something was wrong. By the time my mind processed that I could cross the road, the signal changed. On my physician’s recommendation (a gentle, calm and very caring man who doubled as my Psychologist for the first few months), I tried using simple techniques like following other people whenever I could or using the skyways and subways.
Aphasia (Transcortical Sensory)
Aphasia is an impairment of language, affecting the production or comprehension of speech and the ability to read or write.
I couldn’t make conversation without stammering for words especially when I had to talk to one of my colleagues or professors about work. It was as if I forgot all the jargon in my field overnight. I felt very incompetent and unqualified to participate in meetings.
Now, I experience dysphasia due to migraines, side effects of medication, or when I’m very stressed out. The difference is that with aphasia, I didn’t know that there is a word for something or that I know that word. On the other hand, with dysphasia, I know that there is a word for it, and I know that I know it but I can’t remember it just now. I always keep a thesaurus open on my phone to get around dysphasia.
Tinnitus
Tinnitus is the perception of noise or ringing in the ears. My ears would start ringing out of nowhere and it took me a long time to realize that the noise was not external. Sometimes, it would be loud to the point that it hurt and I couldn’t hear anything from outside.
Increased heart rate
My heart rate would randomly go up and I’d hear my heart pounding while I am sitting or watching TV. It would take a while (5-15 min) to go back to normal without any help. I usually did not do anything physically intensive. Increased cholesterol levels may have contributed to fatigue and increased heart rate while taking stairs but nothing explained the increased heart rate while lying down.
Loss of temperature sense
You obviously know where I live and how cold it gets here. I had a minimum to no sensation of cold even during winter and I could not tell how cold it got. I could go out in the snow with no footwear without feeling very cold. Some days, my hands and feet would freeze blue but I could not feel it.
Drooping eyelids
By the time I got operated on, my eyes were half-closed with drooping eyelids. I think it’s a sign of muscular fatigue but in my eyes, it was another thing I was losing control of.
Tingling
I’m not sure if my medication caused it but I’d feel severe tingling in my feet and hands. It’s more of an annoyance than pain because there is nothing you can do with tingling hands and legs.
Blurred vision
I saw shaky things through a misty cloud for a couple of months and it magically cleared up when I woke up from surgery. I get blurry vision when the intracranial pressure increases from lifting weights or migraines.
Constant multiple headaches
For more than 6 months, I could report at least two types of headaches (numbing, pinching, aching, shooting, shocks, pulsating) in two different locations (forehead, temples, top, behind, left-behind, right-behind, top-left, top-right, closer to neck) at any point of time (yes! I could feel even in such deep sleep). I forgot what it is like to not have a headache. A month after the surgery is when my headaches started clearing up and the world suddenly looked so much brighter.
I do experience headaches now and then but they are not so complex and often associated with migraines or strain.
Alexia without Agraphia
Pure alexia, also known as agnosic alexia or alexia without agraphia or pure word blindness, is one form of Alexia which makes up the “peripheral dyslexia” group. Individuals who have pure alexia suffer from severe reading problems while other language-related skills such as naming, oral repetition, auditory comprehension or writing are typically intact.
I could write but not read. I could read out what letters and words there were in the text and even tell what each word meant. But I couldn’t make sense of the words put together. It would take me very long to understand what a paragraph meant and by the time I got to the next paragraph, I’d forget what the previous paragraph meant. A very handsome young neurology resident told me what this condition is called and that I’ve it. He did make it easy to learn by being so cute but living with it in graduate school wasn’t the least bit funny. It was embarrassing and killed my confidence almost instantly because if you aren’t reading, then you’re doing nothing in the life I chose. Now, I only have issues with reading or writing when I have severe migraine attacks.
Sleep Paralysis
Sleep paralysis is a feeling of being conscious but unable to move. It occurs when a person passes between stages of wakefulness and sleep. During these transitions, you may be unable to move or speak for a few seconds up to a few minutes.
I used to have it quite often before surgery. Once or twice even while awake. I was taking a shower one day and realized I couldn’t move anymore. I stood in the bath for almost 30 min and there was nobody in the house I could shout for help. I was so scared that I thought I was going into a coma or something bad was going to happen. But after 30-35 min of being scared for my life, I was able to move. I went out of the bathroom and only saw my roommate’s puppy. So I said, “Bailey, please don’t let me die today.”
I called the emergency line and the nurse practitioner thought I could have had a stroke. So I went to the emergency room but they didn’t see any signs of a stroke. The ER physician contacted my neurologist and neurosurgeon (not the one who removed the tumor). Both asked the ER physician to discharge me and increase the dosage of Diamox (to reduce intracranial pressure).
Depersonalization
Depersonalization-derealization disorder occurs when you persistently or repeatedly have the feeling that you’re observing yourself from outside your body, or you have a sense that things around you aren’t real or both. However, people with this disorder do not lose contact with reality; they realize that things are not as they appear.
As I kept losing control of more and more of my body functions, my consciousness started isolating itself (even from cognition) and looking at my body as a container rather than a wholesome person. It could have also been a coping mechanism to deal with chronic pain and fatigue. It is hard to describe as some of the psychiatric symptoms tend to be philosophical. I don’t know what that feels like anymore but I found this excerpt from my diary entry on 15 Jan 2015:
“I want you to picture this scenario – one of the headlights of your car broke and needs mending. What do you do? Do you stop going to work until you get it repaired? Or do you still keep doing everything as usual and get it repaired when you find the time? I’d assume the latter.
A lot of you have been asking me what it is like to have a tumor. Well, quite similar to the above scenario, only a little different. If you hurt your hand, your brain would know it. But if there is a problem with the brain, I’d know it! The body is very similar to a vehicle – it gives you a physical manifestation, the brain being the control center. The subtle difference is that there is a ‘me’ that the brain belongs to. So, in short, to have a tumor in your brain is like separating your consciousness from the rest of your body and then looking at what it has to offer.”
Trigeminal Neuralgia
I had episodes of severe, shooting, or jabbing pain that feels like an electric shock in my ears. Each episode might last a few minutes and episodes occur close together. Then, I’d go without any episodes for a few months. At first, I thought it was just the nerves regenerating in my ears because I had the same experience with facial nerve regeneration a few months after surgery. But these happen only in my ears and haven’t stopped in two years. Right now, I’m not seeking any treatment for it because it is not so bad that I spent time and effort on pursuing it.
In addition, I also from constipation and loss of libido which are usually caused by most tumors and excessive medication use.
Issues with memory
It is interesting how you can differentiate the different functions of your brain when they are impaired. I could actually understand that I had difficulties with processing information, storing information, retaining information, and recalling information. Even when I could process information with some difficulty, I could not memorize it very well. Remembering and recalling the placement of objects, paying bills, appointments, and other details (both minor and major) of my everyday life was very hard. I think being preoccupied with the notion of getting well helped me get through everyday life but my neuro-psychologist saw it as an impediment to me feeling fine (well, I wasn’t fine and I was not going to let the inadequacy of modern medicine dictate how I feel).
One of the first symptoms I noticed is how impaired my working memory got. I could not remember simple things such as parts of sentences or a 4-6 digit code to copy. This is still an issue in my daily life that keeps popping every now and then. It presents the worst when I try to multitask and push my cognitive abilities. I almost immediately get fatigued and my brain goes into this foggy sleepy mode triggering hypersomnia or a migraine (depending on how well I was doing the previous days).
Chronic Fatigue
If I just as much used my hands, they would start hurting. By using I mean, showering, picking up a purse or eating. My physical exercise consisted of getting up from my bed and walking to the car (I lived in an apartment downtown!). Sitting in the car on the way to the hospital about 5 min away while someone else drove it would drain me out for the rest of the day. It was as if I was exhausted by existing.
If my pre-surgery fatigue was at a 10/10, my fatigue levels right now are at about 1/10. I do get a lot of things done now compared to a few months ago but I still have to go from 6/10 to maybe 10/10 on the energy scale. I do see improvements every few months. Yet, it takes a lot of patience to not be frustrated and disappointed with myself on a day-to-day basis because my life acquires new normalcy every few months and is often different from the previous and vastly different from the one I had before my symptoms started. Regular and controlled exercise helps with improving energy levels gradually but migraines regularly interrupt that and set back my progress.
Neuro-fatigue
Mental fatigue comes in thinking processes, learning and information processing, watching television extensively, doing computer activities, but also solving problems, interpreting the behavior of other people, and thinking logically.
Dizziness
Moving traffic, doorways, patterns on floors or walls, strobes, too much text or information make me feel very dizzy and nauseous. Now, I can handle most of them better quantitatively with the exception of strobes. I recently watched a movie on the IMAX screen and felt fine. Next step – watching a 3D movie!
Pseudobulbar Affect, PBA
Pseudobulbar affect (PBA), emotional lability, labile affect, or emotional incontinence refers to a neurologic disorder characterized by involuntary crying or uncontrollable episodes of crying and/or laughing, or other emotional displays. PBA occurs secondary to neurologic disease or brain injury. Patients may find themselves crying uncontrollably at something that is only moderately sad, being unable to stop themselves for several minutes. Episodes may also be mood-incongruent: a patient might laugh uncontrollably when angry or frustrated, for example. (Source: https://en.wikipedia.org/wiki/Pseudobulbar_affect)
Oftentimes, PBA is confused with depression/anxiety and it goes undiagnosed. I recognized it with a simple test – Do you feel the same way inside and out? In case of depression, you will. With PBA, you often don’t. I’d lie in my bed for hours just staring at the roof without any motivation to get up and do anything, not even eat when I know I’ve been starving. I’d wonder what’s wrong with my motivation and watch TED talks to pick me up. This happened for a couple of months before the headaches or fogginess showed up. It made me question all my life’s decisions (not that I made many by that time :P) although I knew I had a perfect life. It created a constant indifference to everything – to people, to myself, to life in general, and even to death. I felt a state of mind in which sometimes, I would experience neither positive nor negative emotions and the other times, I’d pour my heart out into my diary and cry for hours. A little after surgery, I’d laugh uncontrollably for no reason at all and be embarrassed for doing that.
God bless the people who dealt with my PBA + PMS. You wouldn’t have met a more irrational person in your life! I’m indebted to the victims of my PBA + PMS eternally and love them more than ever.
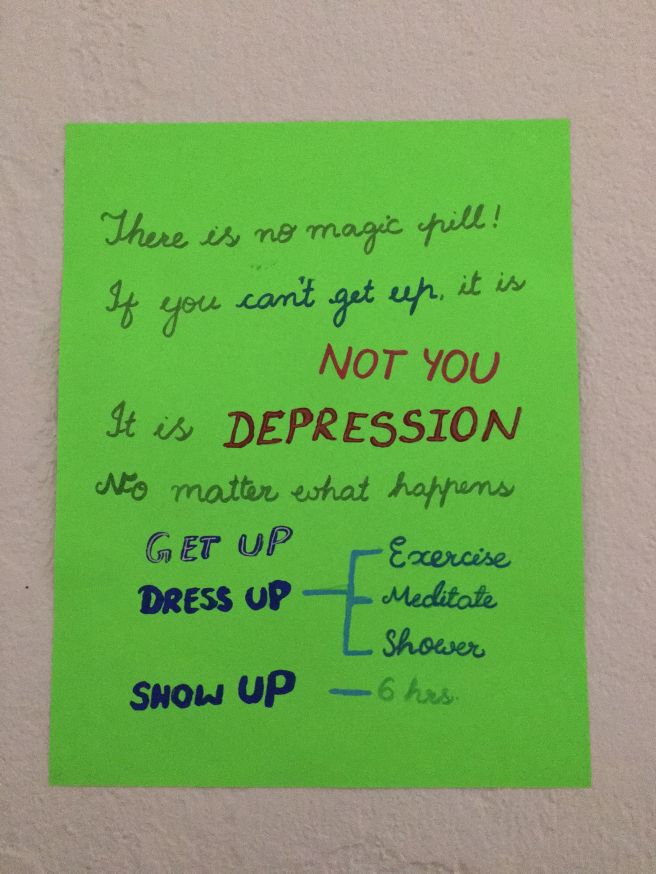
After surgery, the PBA episodes get triggered when I have migraines from pressure/ temperature changes, I exhaust myself physically or mentally, stress, lack of sleep, or a combination of these factors building up. I experience apathy and amotivation for days and random crying episodes intermittently. Though the reasoning in my head says, “Wake up – show up – eat – drink else you will get dehydrated and fall sick – get to work…”, I will have no motivation to do anything. It is a miserable experience to fight this conflict. I feel very embarrassed to go out from the fear of bursting into a crying episode. The crying episodes last between 15- 45 min and the apathy lasts from a few hours to days. A severe episode of PBA leaves me exhausted as if every last ounce of energy has been drained out of my body and lasts for a full week.
Loss of taste sensitivity
Most foods tasted the same except Nutella (of course! :D). Sweet was pretty much the only taste I could decipher. Everything else tasted like nothing.
Brain Fog
I kept complaining to my friends about how I couldn’t think straight. It was like I couldn’t push my thinking beyond a point because my head was in the clouds. This is as accurate as it gets because it’s a very hazy feeling to explain. It was as if I never really woke up completely for more than 6 months. I couldn’t tell reality apart, for example, if you convinced me enough that a certain thing that actually happened, in reality, didn’t happen, I’d believe you because my perception of reality was so limited. My life at that very moment felt surreal and I could never be sure what yesterday looked like. Now, I usually have brain fog in combination with migraines or PBA.
I also experience brain fog in two ways – (1) when I feel numb and my brain can’t think (2) there is hyperactivity in my brain and my brain feels like pulp. Although both lead to challenges with critical thinking, the experience is very different. The first one is more physiological and the current migraine medication (Venlafaxine) I’m on helps with that. The second one is
Limp limbs
For more than three months before surgery, I woke up with limp hands and legs that didn’t work until I stayed in bed for a couple of hours (on good days!). If I got up straight away, my legs would buckle on standing or not walking. It was really funny when I said, “My legs aren’t walking yet”. It’s difficult to understand how that works and I did get asked, “How can your legs not walk?”. But they didn’t! It was similar to my hands as they couldn’t grip objects unless I paid attention to not letting go. My legs would work at some point in the day but I mostly lost control of my hands. I couldn’t hold pens or brushes or open water bottles for a long time. Sometimes, I had to hold one hand with the other to make it sign (which was the only writing I’d do) but that wouldn’t work for more than 5-10 min. All the table manners I was taught all my life weren’t of much use when I couldn’t hold a knife and fork the right way. On most days, I’d wake up saying, “My hands and legs are not working again today”. Please tell me I’m not the only person who finds it funny. Now, I only experience this when I have severe episodes of migraine.
Psychomotor impairment
I am able to hold a pen and write a page or two on good days. But my handwriting changed due to the loss of dexterity. I can’t write long strokes or cursive smoothly anymore. I still cannot hold a thin paintbrush and draw straight lines or paint on a small area. On other days (randomly sometimes), I cannot hold a pen and write a paragraph. My hand hurts severely (as if the nerves are pulling back and muscles are cramping) when I try to force it to write before giving up completely.
I didn’t know for more than two years that I also had psychomotor impairment in my left hand. Because I’m right dominant, I only noticed that I can’t do things with my right hand as well as I used to. It was only when I got a neuropsychological assessment that I found out that my left hand is more impaired than the right. The neuropsychologist was surprised at how someone couldn’t notice this level of impairment.
Challenges with balance
Three months after surgery, I got tested for balance and found out that the left side is worse than the right. I’ve been working on exercises for improving balance. I didn’t get an assessment but I think the balance on my right side is back to normal. For the first time in more than 4 yrs., I was able to do a yoga posture balancing on the left recently and that is a huge improvement for me.
Misfiring fingers
“I did type by a ‘p’ this time. Why does it show an ‘i’?”
“I’m very sure I moved it sideways. Why did it move downwards?”
My fingers weren’t listening to me. I also noticed it when playing games on my phone because they move sideways instead of down. It took me very long to type because it required conscious control of my hands and looking at every key and sometimes, using one hand to make the other hand type. Now, I only present this symptom when I have a migraine, try to push my cognitive abilities, multitask, or try to do things quickly rather than at a steady pace (ex., when I try to type quickly at my pre-injury, my fingers start misfiring and soon, my hands become limp).
Irregular Sleep
From mid-September’14 and I suddenly started experiencing somnolence, sleeping irregularly, and continued just sleeping for the next six months. I’d sleep for more than 15 hrs a day and wake up sleepy and fatigued. There were days when I slept for more than 20 hrs, woke up only to eat what’s on the kitchen counter, and went back to sleep. Most days, I’d have no idea which day it was because I would have been sleeping. The only times, I kept myself awake was when I had to go meet doctors because I had to do something to entertain myself apart from sleeping. It was as if I was sleeping for all five years and I got such deep sleep I never even had dreams. I used to feel extremely drowsy even during the few waking hours I had.
I try to get 7.5 – 9 hrs of sleep every night and take a 30-45 min nap in the afternoon. Because I’m still recovering, I don’t mind getting some extra sleep if my body needs it. Sometimes (not always), sleep is the only thing that makes me feel better. Migraines still throw me off balance and make me switch between hypersomnia and acute insomnia. Insomnia causes very bad headaches, irritability, and nausea all day. Now, I cannot function if I didn’t get enough sleep the night before. You’d think hypersomnia would make me feel recharged but it makes me feel fatigued, drowsy, and gloomy.
So please take it from someone who has been on the extreme ends of the spectrum – get enough sleep, there is nothing in the world that can’t wait until tomorrow. Sleep regulates most of the cycles in your body. So if you don’t or can’t get enough sleep, get help immediately!
Sweet Cravings
I don’t know if it was my body compensating for the lack of serotonin(one of the four happy hormones) but I used to physically crave anything sweet. The pineal gland is responsible for the secretion of melatonin, a serotonin-derived hormone that is responsible for regulating sleep cycles. I’m not sure how but my pineal gland got confused and secreted a lot of melatonin putting me to sleep all the time. I think I was low on serotonin which in addition to not making me happy, gave me insatiable sweet cravings. God bless the chap who invented Nutella. I’ve no clue how many jars I finished. Post-surgery, I crave sweets after migraines due to adrenaline fatigue leading to hypoglycemia. Fatigue also makes me preoccupied and desperate for sugar. It has been very difficult to get this urge under control.
Irregular appetite
My hunger cycles were very confusing! For a few weeks, I wouldn’t be hungry at all. The thought of food would make me feel nauseated. A few weeks following that would be days of constant hunger pangs. I’d be hungry even while I’m eating and nothing would satiate my hunger, not even a litre of water. I’d be hungry through day and night and eat everything in my sight.
Currently, the cycles are not that long. They are centered around the migraine cycle with the beginning of migraines coinciding with nausea, acute insomnia, and aversion to all food and sweet cravings, insatiable appetite, and hypersomnia coinciding with ongoing or end of a migraine.
Light Sensitivity/ Photophobia
I couldn’t see any bright lights be it natural or artificial. Neon lights cause headaches, dizziness, and nausea and I couldn’t attend classes or meetings due to that. I used to sit in dark rooms for days because I couldn’t go out to see even daylight. I could not wear any glasses because the weight of the frames caused a lot of pressure to build up.
After surgery, I use indoor and outdoor migraine glasses to cut out artificial and natural light (https://www.theraspecs.com/). I don’t need to constantly wear them now but I always carry both pairs. I can even watch 2-D movies on standard screens now (no 3-D or IMAX).
Auditory Sensitivity
Any sounds used to cause extreme headaches and confusion, even conversations. I couldn’t use a phone to my ear. I could only take calls on the loudspeaker with the least volume level. Any music or TV or sometimes even people talking loudly or quickly caused a lot of dizziness and annoyance. I couldn’t walk on a street or stay in any public spaces like restaurants for long. People talking inside a car was very difficult to tolerate. Going to a party or a movie was out of the question.
I got much better with the noise sensitivity – I can now sit through a movie and even a party without loud music for a couple of hours. But I always carry earbuds in case I need to block out some noise and prevent over-stimulation.
Nausea
Nausea and headaches worsened each other. I had constant nausea for almost six months. After my initial diagnosis, I was on constant medication to reduce nausea so it wouldn’t lead to vomiting, dehydration, or worsening headaches. I took medication for nausea after each meal. Any change in pressure, temperature, motion, altitude, or medication worsened nausea.
Now, I have nausea from migraines and medication which occasionally leads to vomiting. But I am not on medication anymore.
Problems with Comprehension
It first started with the inability to read (see pure alexia) and then progressed to me not being able to understand normal conversations. Irrespective of language, I couldn’t comprehend language, sounds, visual signals, or even touch effectively. Sometimes, there was a delay in comprehension, other times, just dizziness and brain fog. I couldn’t attend meetings or classes and make sense of what people said. I couldn’t be a part of conversations that had more than one person (other than me). I could only understand if the other person spoke at a lowered pace and voice. I had to record all my doctors’ appointments and listen to them later to make sense of them. I couldn’t understand or learn new information well.
I still have problems with comprehension when I’m stressed or exhausted. It usually presents as brain fog first.
Head Pressure
Although everybody experiences a head rush from getting up or bending down too quickly, I have to be more careful to make sure the head rush doesn’t increase too much pressure in my brain as it puts me down for days. I get increased head pressure from
- lifting weights (> 15 lb below shoulder level and >6 lb above shoulder level)
- increase in blood pressure (from medication)
- increase in blood circulation to the brain (from bending or activity)
- multitasking (ex., driving)
- bicycling (I’m able to ride a stationary exercise bicycle at a slower speed now)
Increased head pressure puts me down for days. It causes instant neuro fatigue (in less than 10 min. after activity) and drowsiness. It usually takes 3-5 days to recover and I often don’t understand it immediately.
De-regulated Metabolism
The injury caused by the tumor and surgery resulted in extreme weight gain, vitamin deficiencies, abnormal lipid panel, and hormonal imbalances (testosterone, estrogen, serotonin). I gained 30 lbs in a year through diagnosis and a few months after surgery. Due to fatigue and amotivation, I could not focus on getting enough exercise for a long time.
I am now trying to improve my metabolism and reduce inflammation in my body through healthy food and exercise. I had to take a very high dosage of supplements for vitamin D (60,000 IU) for a few months. But apart from that, I am just being patient with my body to return to its original state.
Water retention
Any change in medications or living conditions causes my body to retain water and plump up like a balloon. It also goes down by itself as my body gets used to the new conditions but it is bothersome when traveling (when my clothes or finger rings don’t fit) or people around me say I gained more weight (shakes my self-confidence). I had to take medication only once so far on a month-long trip.
This is one of the visual symptoms. Although invisible illnesses are hard to live with (some people do say things like, “You look fine to me”), visible symptoms are equally annoying because it is hard for others to empathize with your struggle underneath. I’m fortunate to have as much support as I do from friends, family, and the workplace. It is still hard for them to empathize with something that is unfathomable.
Swelling of neck
Whenever I experience stress or strain, the intracranial pressure increases causing my neck to swell up. It causes increased headaches and a feeling of heaviness in my head as if a huge rock is sitting on top of my neck. I don’t have a diagnosis of IIH (Idiopathic intracranial hypertension) but mild symptoms related to it are common after craniotomy. It also triggers some of my cognitive symptoms such as comprehension problems.
Restless Leg Syndrome (RLS)
Restless legs syndrome (RLS), also called Willis-Ekbom Disease, causes unpleasant or uncomfortable sensations in the legs and an irresistible urge to move them. Moving the legs or walking typically relieves the discomfort but the sensations often recur once the movement stops. Symptoms commonly occur in the late afternoon or evening hours, and are often most severe at night when a person is resting, such as sitting or lying in bed. Since symptoms can increase in severity during the night, it could become difficult to fall asleep or return to sleep after waking up. RLS is classified as a sleep disorder since the symptoms are triggered by resting and attempting to sleep, and as a movement disorder since people are forced to move their legs in order to relieve symptoms. It is, however, best characterized as a neurological sensory disorder with symptoms that are produced from within the brain itself. (Source: https://www.ninds.nih.gov/Disorders/Patient-Caregiver-Education/Fact-Sheets/Restless-Legs-Syndrome-Fact-Sheet)
I had severe RLS in my insomnia days which in turn made it worse. Now, I experience it when I’m sleep-deprived, exhausted (physically, mentally, or emotionally), or don’t get enough exercise. Migraines, limp limbs, and RLS play against each other and I dread having to deal with them at the same time. The only thing that helps (sometimes) is a heat pack on my legs.
Migraines
Migraines are the most debilitating result of brain injury and they are triggered by any or combination of a number of triggers:
- Dehydration
- Sudden temperature change
- Barometric pressure change
- Altitude change
- Sleep deprivation & jet lag
- Physical exertion
- Overstimulation (any sensory)
- Low/ high humidity (than average)
- Caffeine (this has been getting better)
- Excessive mental activity
- Stress
- Emotional exhaustion
- Menstruation
Often, they cause brain fog, comprehension problems, chronic fatigue, limp limbs, irregular sleep cycles, PBA, nausea and vomiting, and drowsiness. My scalp also becomes very sensitive and tender and hurts when I touch my hair. In spite of keeping it short, my head and hair feel very heavy during migraines.
With chronic conditions like migraines, life feels like just surviving every day rather than living without fear. My daily life is severely limited by migraines because so I couldn’t find any medication that worked so far. Thunderstorms are my worst fear as they incapacitate me for days. Before starting my current medication regimen, I was non-functional for 22-25 days a month because I spent most of those days sleeping or in pain. I can’t even watch TV on severe migraine days as my comprehension levels and threshold for sensory stimulation are very low.
I started taking a daily prophylactic (Venlafaxine 150 mg ER) for migraines after trying to deal with it naturally for almost a year and a half. Then, I added getting botox every quarter and Emgality (we still need to know the long-term effects) every month. I also take magnesium, coq10, and melatonin (0.3 mg) supplements to improve my threshold to migraines. In the past, I got acupuncture for pain but the relief was very short-term. After adding this regimen, I still have 5-7 non-functional days per month but my quality of life on other days improved enormously.
Although these are effective in reducing the intensity, I made a lot of lifestyle changes:
- balancing the amount of activity each day (I have learnt to say no to things that might create stress or require a lot of physical or mental activity. Although being in graduate school is like punching my brain with no routine and critical thinking day-in and day-out, I try to balance it out with days of easy and hard tasks)
- working out every day (I have been doing yoga thrice a week)
- hydrating through the day
- staying in temperature, pressure, and noise controlled environment (reduce sensory overload as much as possible. This is the hardest and sometimes, impossible to do)
- eating fresh vegetables and fruits
- sleeping 7-9 hrs every night and taking a nap in the afternoon as needed (listening to my body when it needs more sleep helps me from getting a migraine attack before I recuperated from the previous one)
- reduce sugar and salt intake (I don’t buy lunch meats or ice cream anymore)
- avoiding caffeine after 2 PM (I stopped drinking coffee after surgery. I only have green tea or matcha once or twice a week.)
- reducing icy drinks or foods (I always ask for hot water at restaurants. Ice water gives me an instant headache on most days.)
- reducing stress as much as possible (This has been almost impossible as it is easy to get overwhelmed from overstimulation or being unable to function at a normal pace due to the impairments. I try to meditate every day to reduce stress but it still remains the worst trigger of all.)
Loss of Hearing
Due to the noise sensitivity, I didn’t know I was losing hearing in my right ear. This was one of the early symptoms as I found out (incidentally!) that there was a slight difference between my left and right ears a year and a half before my diagnosis. But the physician just said this may be due to using a phone or headphones for long periods of time. At that time, he only diagnosed decreased sensitivity in hearing in my right ear. I did follow his advice but the hearing in my right ear only worsened till surgery. The actual hearing loss was again, an incidental finding during one of my neuro ENT visits.
There is a drastic difference in hearing between my ears but I couldn’t tell the difference until the sensitivity got better several months after surgery. I have moderate to severe conductive hearing loss in my right ear which I’ve been told will not reverse. But because it has been stable for two years now, I’ve been advised to get a surgery to reverse the damage caused by the tumor. Although it doesn’t bother me in daily life, if I don’t use that part of my brain for an extended period of time, it might increase my risk for dementia.
Issues with visual focus
My eyes have difficulty focusing together when my brain is under any kind of stress. Right now, I wear glasses that have higher power than I need to reduce that strain on optic nerves to focus. It is surprisingly effective and a lot cheaper than prism glasses or vision therapy (which I’ve been advised if the focus gets worse).
Floaters in eyes
This is the strangest thing that the pineal tumor caused. Most of my cysters say that their floaters coincided with brain injury symptoms too but no one has an explanation for it. They don’t bother me so I don’t plan to do anything about it currently.
Amnesia
Retrograde amnesia is a loss of memory access to events that occurred or information that was learned, before an injury or the onset of a disease. “This is the kind of amnesia that is most often dredged up as a plot element in bad comedies and cheap mystery stories; so-and-so gets hit on the head and then can’t remember who he is anymore, wanders around aimlessly, finding himself in zany predicaments, until he gets hit on the head again and his memory remarkably returns. This almost never occurs in real life. Although retrograde amnesia is real, it’s usually the result of a tumor, stroke, or other organic brain trauma. It isn’t restored by a knock on the head. Because they can still form new memories, patients with retrograde amnesia are acutely aware that they have a cognitive deficit, are painfully knowledgeable about what they are losing.”
I lost memories of the visuals of most of my life before surgery which caused derealization. I know the story of my life broadly but it is as if there is a distance between me and my life before surgery. I do regain some of them randomly or when I re-visit some places. I did forget a few people’s faces and a lot of places (my college :O). There are things (ex. music) I like but not sure why or from when. Because I lost most of the visuals, I don’t feel very emotional about incidents in my past. I have difficulty feeling emotionally connected to the people I knew in the past. It causes a lot of emotional conflicts constantly interfering with re-inventing identity after injury. I mostly have emotional memory loss but some episodic memory loss too. I lost a lot of happy memories but then, I am not hurting from any of the sad memories either. One of my friends who also suffered from amnesia said, “You have a life now and plenty of time to make new memories. Don’t worry about what is gone. You can be the person you want to be rather than the one you were.” The curiosity to piece my life together from snippets I hear from people never dies. But then, human memory is faulty. I hear different versions of the same story from different people. Other times, I have a gut feeling that the story is not quite right but I don’t know what the actual story is. Listening to someone talking about past incidents I don’t remember gives me a bad headache instantly.
Scars
I have a prominent surgical scar and a dent in the back of my head. It is not visible from the hair but it took a long time to heal. I keep my hair short so that the hair doesn’t pull the skin around my scar and make it sore. Although it healed and the scar formed, it doesn’t take much for the scalp in that area to get sore and sensitive to touch.
Note: This is a living breathing document. It will change!